Again and again, studies have shown that doctors tend to make clinical decisions for patients based on how much they themselves will get paid.
In 2007, we learned from the COURAGE trial that angioplasty and stents—percutaneous coronary intervention (PCI)—don’t reduce the risk of death or heart attack, but patients didn’t seem to get the memo. Only 1 percent realize there was no mortality or heart attack benefit, perhaps because most cardiologists fail to mention that fact. One can imagine that if patients actually understood that symptomatic relief was all they were going to get, with “no additional mortality benefits,” they’d be less likely to go under the knife. Then, ten years later, the ORBITA trial was published, showing even the promise of symptom relief was an illusion.
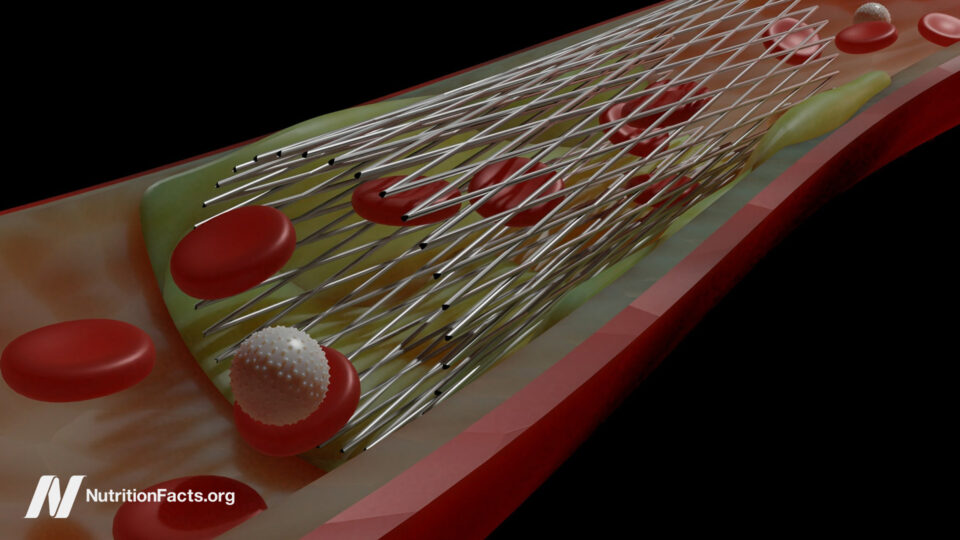
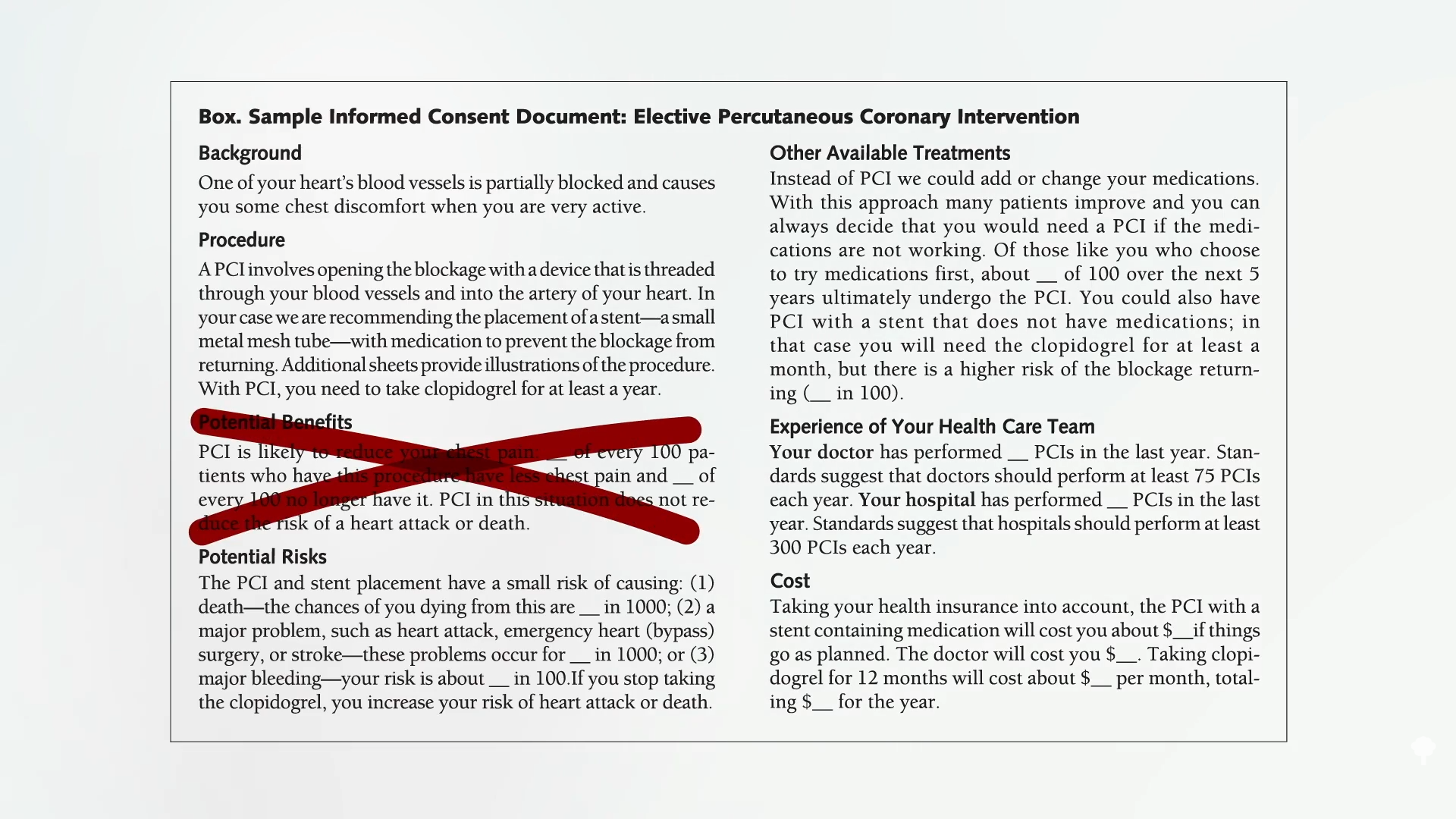
“The implications of ORBITA are profound and far-reaching. First and foremost, the results of ORBITA show unequivocally that there are no benefits for PCI compared with medical therapy for stable angina,” that is, heart disease. Basically, patients would be risking “harm for no benefit. It is hard to imagine a scenario where a fully informed patient would choose an additional invasive treatment for no added benefit.” Remember the stent consent form I discussed previously, shown below and at 1:17 in my video Why Are Stents Still Used If They Don’t Work?:
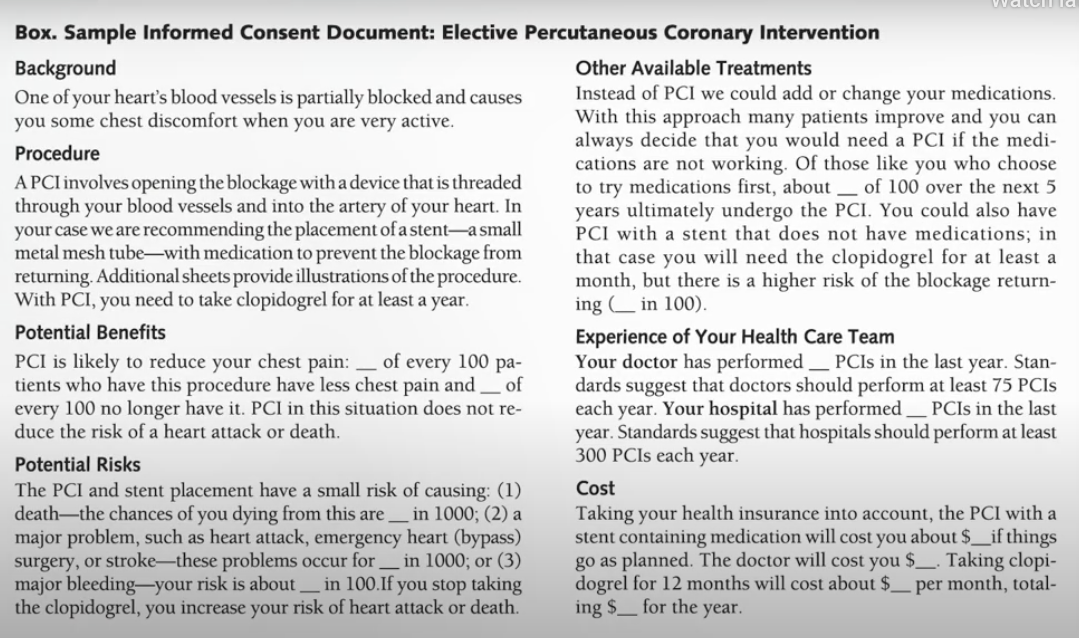
Now, it looks like this, seen below and at 1:21.
So, is the ORBITA trial the “last nail in the coffin for PCI in stable angina?” That is, for stents in non-emergency situations? An editorial in the journal Cardiovascular Revascularization Medicine disagreed, pointing to “the broad angina relief that occurred in both arms.” In other words, stents helped—even if the sham operation without stents helped just as much. So, “if the patient is treated with PCI and is benefiting from the ‘placebo effect,’ who am I to interfere with that benefit of this ‘therapy’?” In that case, why not perform fake surgeries? Stent placement can cost around $40,000. It’d be cheaper to just fake it all. The reason we shouldn’t keep electively stenting people is because there’s a body count. During stent placement, 2 percent of patients develop bleeding or blood vessel damage, while another 1 percent die or have a heart attack or a stroke. And because something is stuck in your chest, 3 percent of patients have a bleeding event from the blood thinners that must be taken. Or the blood thinners don’t work and the stent clots off and causes a heart attack.
Why are they still done when we not only don’t have evidence of benefit but, in many cases, we have explicit “evidence of no benefit”? One of the sources of resistance may be all the financial gain. These procedures make a lot of money for hospitals. Don’t expect them to begin promoting “lifestyle changes to combat heart disease. Nor will physicians quickly abandon a practice that both supports their income and seems to make sense.” Is it that simple? Is it that famous Upton Sinclair quote: “It is difficult to get a man to understand something when his salary depends upon his not understanding it.” Think that’s just cynicism? Let’s ask doctors themselves.
Thousands of physicians were surveyed, and 70 percent “believed that physicians provide unnecessary procedures when they profit from them.” That’s what doctors themselves believe. And the data bear this out. Doctors have been shown to make clinical decisions for patients based on how much they get paid. For example, when choosing which chemotherapy to treat breast cancer, increasing a physician’s margin by 10 percent can yield up to a 177 percent increase in the likelihood of choosing one drug over another.
That may be why Caesarean sections “are more likely to be performed by for-profit hospitals as compared with non-profit hospitals.” “Operating on commission.” Pay surgeons per procedure, and you can increase surgery rates by 78 percent. Could that explain why we do 101 percent more angioplasties than any other affluent country? A study on “physicians’ financial incentives and treatment choices in heart attack management” found that they do indeed “respond positively to the payments they receive and that the response is quite large…Unconditionally, plans that pay physicians more for more invasive treatments are associated with a larger fraction of such treatments,” seeming to result in more invasive treatments. So, it may actually be quite common for patients to receive different treatments based on whether the doctor is getting paid per procedure.
One of my heroes, Dr. Caldwell Esselstyn—who always tries to see the best in people—had to admit that compensation may be playing a role. Evidence surfaced that “doctors have run up millions of dollars in medical bills by doing unnecessary stent implants,” doctors like Mark Midei who inserted 30 stents in a single day. That could be about a million dollars worth of billing. As a token of gratitude, a sales representative from the stent company spent more than $2,000 to buy “a whole slow-smoked pig, peach cobbler, and other fixings for a barbecue dinner at Dr. Midei’s home.”
“The US is just about the only developed country where health care is delivered on a fee-per-service basis and we very liberally incentivize physicians for doing invasive procedures,” explained the chief of cardiovascular medicine at the Cleveland Clinic. “The economic incentives are just too strong.”